Understanding Hysterectomy Risks: A Comprehensive Guide for Women's Health
When considering a hysterectomy, it's crucial for women to understand the potential risks involved. As a major surgical procedure that involves removing the uterus, a hysterectomy can significantly impact a woman's health and quality of life. Proper knowledge empowers women to make informed decisions in collaboration with their healthcare providers. This comprehensive guide explores the various hysterectomy risks, factors influencing these risks, and advancements in medical practice aimed at minimizing complications.
What Is a Hysterectomy?
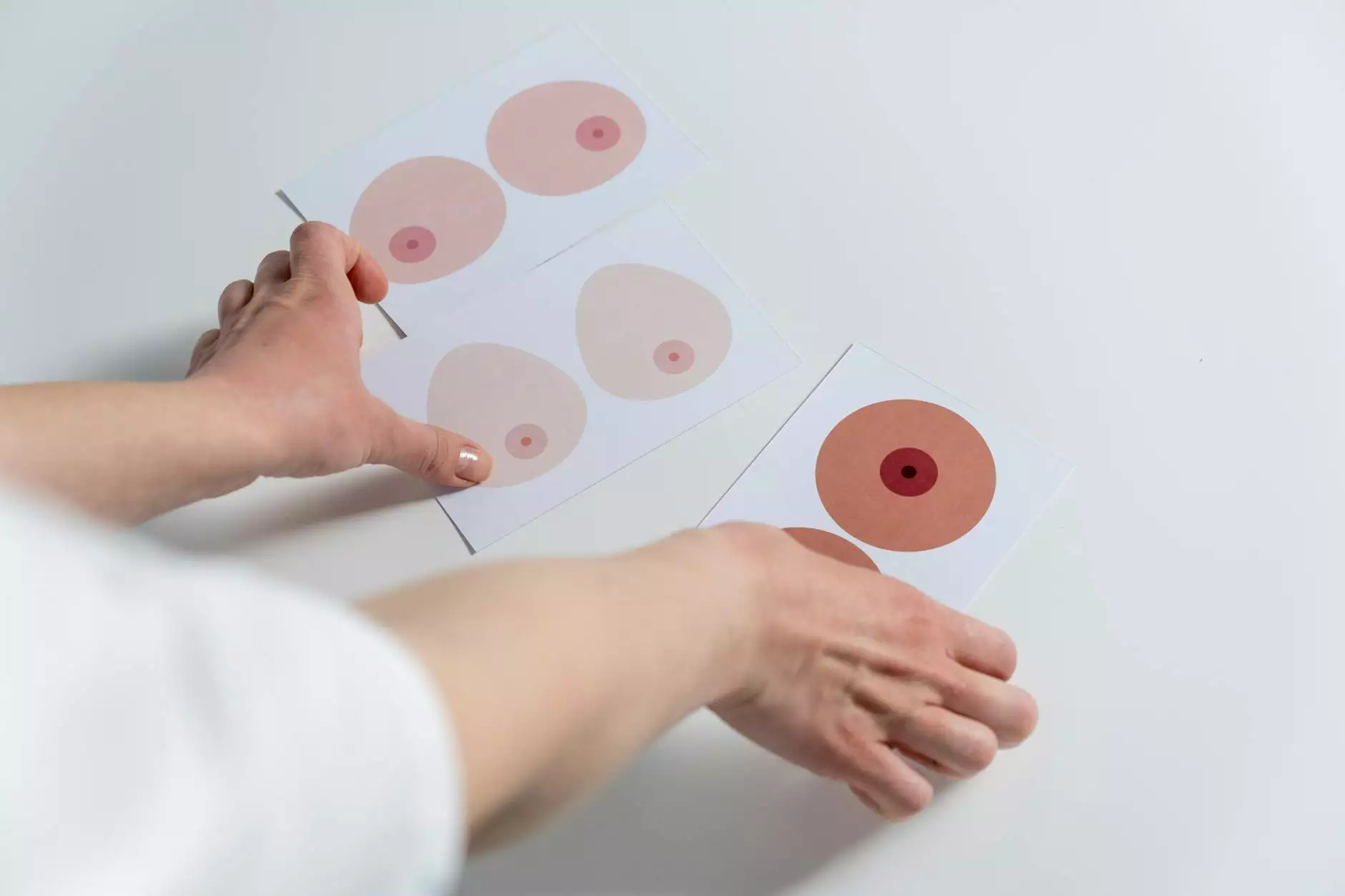
A hysterectomy is a surgical procedure that involves the removal of the uterus, and sometimes surrounding tissues and organs, depending on the medical indication. It is commonly performed to treat conditions such as fibroids, endometriosis, uterine prolapse, abnormal bleeding, or cancer of the reproductive organs. Types of hysterectomy include:
- Subtotal (Partial): Removal of the upper part of the uterus, leaving the cervix intact.
- Total Hysterectomy: Removal of the entire uterus and cervix.
- Radical Hysterectomy: Removal of the uterus, tissues around the uterus, part of the vagina, and possibly lymph nodes—typically used in cancer treatment.
Each type has specific indications and varying risk profiles. The decision to undergo a hysterectomy depends on multiple factors, including the patient's overall health, specific condition, and personal preferences.
Understanding Hysterectomy Risks: What Every Woman Should Know
Like any major surgical procedure, a hysterectomy carries certain risks and potential complications. It's essential to evaluate these risks in context and discuss them transparently with your healthcare provider. Below, we detail the most common and significant hysterectomy risks.
Immediate Surgical Risks
These are complications that can occur during or shortly after surgery, and include:
- Bleeding: Excessive blood loss during or after the operation may require transfusion.
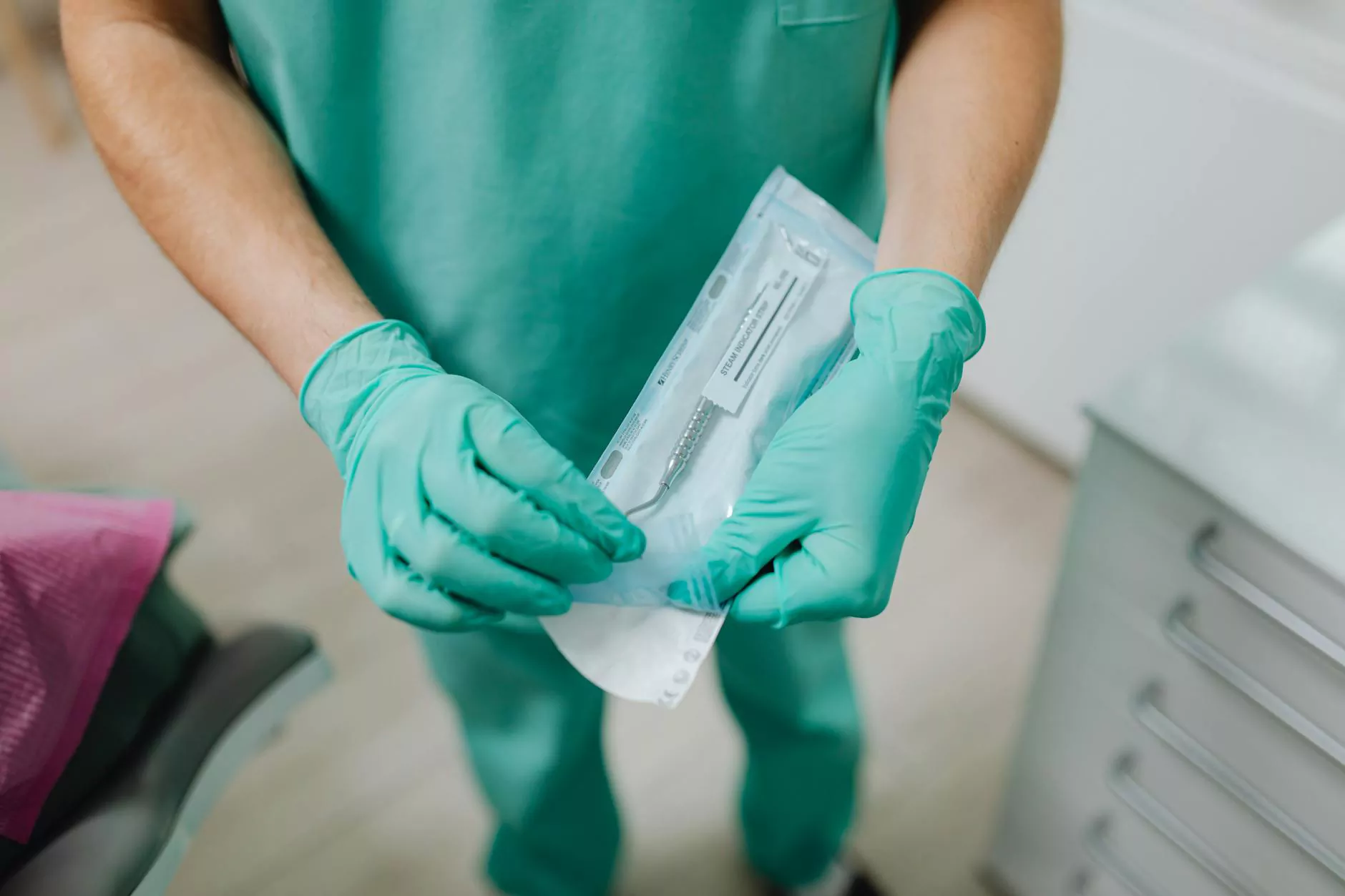
- Infection: Surgical site infections are possible despite strict aseptic techniques.
- Damage to Surrounding Organs: The bladder, ureters, or bowel may be inadvertently injured, leading to further medical interventions.
- Anesthesia Complications: Reactions to anesthesia drugs can occur, though rare with modern practices.
- Blood Clots: Formation of clots in the legs (Deep Vein Thrombosis) or lungs (Pulmonary Embolism).
Long-term Hysterectomy Risks
Beyond the immediate postsurgical period, women must be aware of potential long-term implications, including:
- Hormonal Changes: If both ovaries are removed (oophorectomy), women experience sudden menopause, leading to symptoms like hot flashes, mood swings, and increased cardiovascular risks.
- Osteoporosis: Loss of estrogen accelerates bone density loss, increasing fracture risk.
- Sexual Function Changes: Some women report decreased libido, vaginal dryness, or discomfort, although experiences vary widely.
- Emotional and Psychological Effects: Feelings of loss or depression can occur, particularly when hysterectomy is performed to treat cancer or severe disease.
- Risk of Pelvic Floor Dysfunction: Alterations in pelvic support structures may lead to prolapse or incontinence over time.
Specific Risks Related to Surgical Approach
The method of hysterectomy—abdominal, vaginal, or laparoscopic—also influences risk profiles:
- Open Abdominal Hysterectomy: Higher risk of wound infection, longer recovery, and more postoperative discomfort.
- Vaginal Hysterectomy: Generally less invasive with fewer complications but not suitable for all cases.
- Laparoscopic or Robotic Hysterectomy: Reduced recovery time and fewer incision-related complications, though potential for specialized risks like trocar site hernia or nerve injury.
Factors Influencing Hysterectomy Risks
Several variables can modify the likelihood and severity of hysterectomy risks. Understanding these helps in surgical planning and outcome optimization:
- Patient’s Age and Overall Health: Younger women in good health tend to experience fewer complications.
- Underlying Conditions: Certain chronic diseases such as diabetes or hypertension increase perioperative risk.
- Surgical Complexity: Extensive procedures or presence of severe pathology increase risk levels.
- Surgeon’s Experience: Specialized and experienced surgeons typically have lower complication rates.
- Preoperative Planning: Proper imaging, assessment, and preparation reduce intraoperative surprises and complications.
Advances in Medical Technology: Minimizing Risks
The field of gynecologic surgery has evolved significantly, resulting in advances that reduce hysterectomy risks. Notable developments include:
- Minimally Invasive Techniques: Laparoscopic and robotic-assisted surgeries offer smaller incisions, less pain, and faster recovery.
- Enhanced Imaging: Better preoperative diagnostics assist in precise surgical planning.
- Precision Surgical Tools: Advanced cautery, energy devices, and suturing systems optimize tissue handling and reduce injury.
- Improved Anesthesia and Pain Management: Better techniques minimize anesthesia-related risks and postoperative discomfort.
- Multidisciplinary Teams: Collaboration among specialists ensures comprehensive management of complex cases.
Preoperative Preparation for Reducing Hysterectomy Risks
Preparation plays a benchmark role in mitigating hysterectomy risks. Key steps include:
- Comprehensive Medical Evaluation: Screening for infections, anemia, and chronic conditions.
- Patient Education: Clear understanding of procedure, risks, and postoperative expectations.
- Optimizing Underlying Conditions: Managing diabetes, hypertension, or other diseases preoperatively.
- Lifestyle Modifications: Encouraging smoking cessation, weight management, and physical activity.
- Psychological Support: Addressing fears or anxiety related to surgery.
What to Expect Post-Hysterectomy
Postoperative care is vital to reduce complications and ensure smooth recovery:
- Pain Management: Proper medications and rest.
- Wound Care: Keeping incision sites clean and dry.
- Monitoring for Complications: Watching for signs of infection, bleeding, or organ injury.
- Follow-up Appointments: Regular check-ups to assess healing and address concerns.
- Emotional Support: Counseling or support groups if emotional or psychological issues arise.
Conclusion: Making Informed Decisions for Women's Health
Understanding the intricacies of hysterectomy risks allows women to approach the procedure with confidence and clarity. Advances in surgical techniques and preoperative care have markedly reduced many complications, but awareness remains essential. Consulting seasoned specialists like the team at drseckin.com, who specialize in Doctors, Health & Medical, Obstetricians & Gynecologists, ensures personalized and safest care possible.
Empowered with knowledge, women can make decisive, informed choices tailored to their health needs and life goals. Whether considering a hysterectomy for medical reasons or exploring alternatives, comprehensive understanding of hysterectomy risks helps in achieving optimal health outcomes.